According to the World Health Organization (WHO), physical inactivity is one of the leading causes of noncommunicable diseases (NCDs), including heart disease, diabetes, and various cancers. Regular physical activity can reduce the risk of heart disease and stroke by 19%, diabetes by 17%, and depression by 28–32%. In addition to the health benefits, WHO estimates that 4–5 million deaths per year could be avoided if more people adopted active lifestyles.
The NHS can learn several key lessons from the Dutch healthcare system, including the importance of clear distinctions between levels of care, which can enhance resource efficiency and improve patient outcomes. Additionally, adopting a more integrated model that emphasizes specialized care and patient well-being could significantly enhance the effectiveness of the NHS.
The economic impact of physical inactivity is staggering. The WHO predicts that, between 2020 and 2030, nearly 500 million new cases of preventable NCDs will occur globally due to inactivity, costing the healthcare system $300 billion in direct medical expenses. These numbers don’t even account for the indirect costs associated with lost productivity.
Current NHS Expenditure on Preventable Conditions
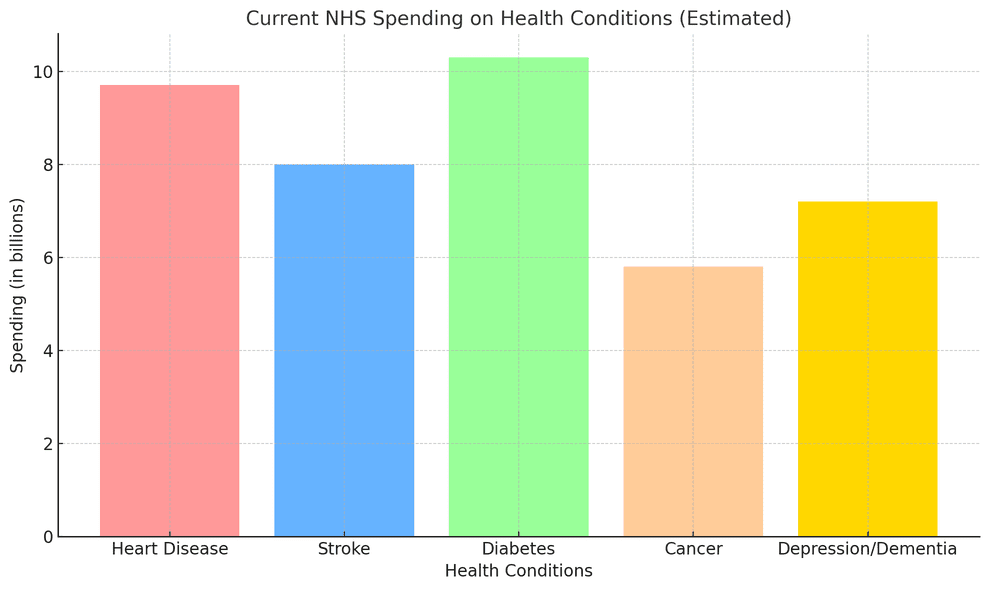
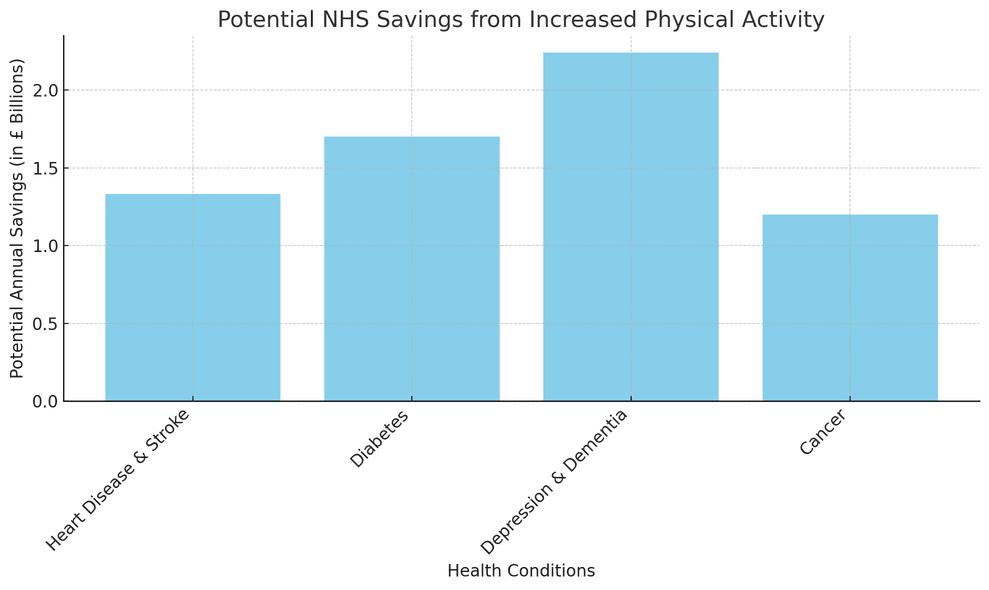
If more people in the UK adopt electric bikes as part of their daily routines, the potential for improving physical activity levels and reducing healthcare costs is significant. By encouraging cycling, we could help mitigate these preventable diseases, ultimately saving the NHS millions each year, maybe even billions there are some differences between the Dutch system and UK NHS though.
Comparing Dutch and NHS Healthcare Systems
When we look at the Dutch healthcare system, what stands out is its structured division into primary, secondary, and tertiary levels of care. This organization is designed to optimize patient pathways, ensuring that individuals receive the most appropriate care according to their specific health needs.
For instance, patients must see a general practitioner (GP) first, who then refers them to a specialist if necessary. This process not only streamlines care but also helps manage resources effectively, as specialists are reserved for more complex cases. Conversely, the NHS operates under an open-access system. Patients can seek hospital-level care without stringent gatekeeping, which provides immediate access but can lead to challenges in resource allocation and continuity of care.
These different access models reflect broader funding approaches in each healthcare system.
The Dutch system is characterized by mixed funding—relying on both taxes and mandatory insurance—which encourages a blend of public oversight and private sector efficiencies. Citizens are required to purchase health insurance from competing providers in the private market, fostering competition and innovation while ensuring universal coverage. In contrast, the NHS is primarily tax-funded, leading to a centralized approach where everyone pays into the system through taxation, making healthcare services free at the point of use. While this model promotes equity and accessibility, it can sometimes struggle with funding adequacy during times of increased demand.
As we continue examining these systems, we recognize that they prioritize different aspects in terms of healthcare delivery.
A key difference lies in their emphasis on efficiency versus comprehensive care. The Dutch system places a premium on efficiency and specialization; there’s a systematic evaluation of healthcare performance metrics that drive quality improvement initiatives. In doing so, they often excel in areas such as patient satisfaction and health outcomes. On the other hand, the NHS prioritizes providing comprehensive care that is accessible to all citizens. This commitment embodies the principle that healthcare should be available without financial barriers—a hallmark value of the British welfare state.
Another noteworthy distinction relates to preventative care strategies.
In the Netherlands, though there is some focus on preventative measures, reimbursement for such services has historically been limited compared to what we might see in the NHS. The NHS actively invests in preventive initiatives aimed at improving population health—think smoking cessation programs or obesity prevention campaigns—which help reduce long-term costs associated with chronic diseases. This proactive approach extends beyond individual patient interactions to community health standards.
Here’s how these priorities play out:
| Healthcare Priority | Dutch Healthcare System | NHS (UK Healthcare System) |
|---|---|---|
| Efficiency | Strong focus on measurable outcomes | Emphasis on broad accessibility |
| Specialization | The high degree of specialization among providers | Generalist care is widely available |
| Preventative Care Approach | Less integrated into standard reimbursements | A central feature of service strategy |
Gaining a deeper understanding of these systems opens up further exploration into structural variations that shape their unique operational landscapes.
Key Structural Differences
Three-Tiered Care in the Netherlands
The Dutch healthcare system is characterized by a three-tiered model that effectively acts as a gatekeeper to specialized medical services. In this framework, primary care providers—like general practitioners—are the first point of contact for patients. In most cases, we must obtain a referral to access secondary or tertiary care. This structure serves dual purposes: it optimizes healthcare resources and ensures that only the most complex cases reach the university hospitals.
While this method fosters a sense of efficiency, it might delay timely care for conditions that require immediate attention. Picture someone needing an urgent specialist—the extra step of going through their primary care doctor could mean longer waiting times. However, the philosophy behind this approach centers around cost-effectiveness and preventing unnecessary visits to high-level specialists.
NHS’s Open Access Model
In stark contrast, the National Health Service (NHS) employs an open access model that allows patients to seek care directly from hospitals without the need for referrals. This model prioritizes accessibility, allowing us to quickly address health concerns as they arise. However, therein lies a significant pitfall: the NHS sees many patients with minor ailments crowding emergency departments meant for critical cases.
The unrestricted access encourages individuals to bypass primary care entirely, leading to overburdened hospitals and wasted resources on treating conditions that could have been managed at the primary care level. As we reflect on our experiences with both systems, it’s evident that while immediate access may seem appealing, it can inadvertently result in inefficiencies and strain on healthcare resources.
By examining these structural approaches, we recognize the balance needed between accessibility and maintaining organized healthcare pathways. Each system has its strengths and weaknesses, prompting us to ask ourselves how we can learn from each other’s experiences to enhance service delivery in our own contexts.
This evaluation sets the stage for a deeper exploration into how different paradigms function regarding public and private sectors in the realm of healthcare.
How Physical Commuting Can Improve Health and Wellbeing in the Workforce
Active travel such as walking, cycling, and the use of electric bikes offers significant health and economic benefits. The shift towards active travel reduces the societal costs of absenteeism, presenteeism (working while sick), and poor productivity. In fact, employees who regularly engage in physical activity are likely to have:
- Lower turnover rates and reduced absenteeism.
- Improved productivity and employee morale.
- Lower healthcare costs for both employers and the NHS.
By promoting active commuting, employers benefit from healthier, happier employees. Electric bikes, in particular, make cycling accessible to a broader audience, encouraging even those who may find traditional cycling challenging.
Improving Air Quality by Walking and Cycling
Air pollution remains a major issue in the UK, contributing to an estimated 40,000 early deaths each year. Road transport accounts for up to 80% of pollution where legal limits are being breached, making it clear that reducing car use is essential.
Shifting from short car trips to walking, cycling, and electric bikes could dramatically improve air quality. The “Avoid, Shift, Improve” model encourages the use of active transport and public transport as viable alternatives.
Cleaner air results in fewer pollution-related illnesses, which could lead to significant savings for the NHS in treating respiratory conditions like asthma and COPD.
The Role of Active Travel in Improving Mental Health
Mental health is a growing issue in the UK, with one in six workers experiencing depression, anxiety, or stress at any given time. Regular physical activity, including cycling, has been shown to have a positive impact on mental health by reducing symptoms of anxiety and depression.
For commuters, switching from driving to cycling or electric bikes not only boosts physical health but also improves mental well-being. Active travel reduces stress and can offer a sense of freedom and control, contributing to better mental health. This, in turn, can alleviate some of the burdens on the NHS by reducing the need for mental health interventions.
Encouraging Widespread Adoption of Electric Bikes
Electric bikes (e-bikes) have the potential to revolutionize how people travel, especially for short and medium-distance commutes. Unlike traditional bikes, e-bikes provide an option for those who may not be physically able or motivated to cycle, such as older adults, those with medical conditions, or those living in hilly areas. The electric assistance reduces the physical effort required, making cycling accessible to more people without eliminating the health benefits.
E-bikes offer a middle ground between sedentary car travel and physically demanding cycling, making them a practical solution for many individuals. A study from Transport for London found that people who switched to e-bikes travelled longer distances than they would on a regular bike while still reaping the cardiovascular benefits of regular cycling.
By incentivizing the adoption of e-bikes through government subsidies or employer programs, the UK could see a substantial increase in physical activity levels across a wider population segment, contributing to lower NHS costs related to inactivity.
Long-term Economic Benefits for the NHS
By incorporating electric bikes into daily routines, not only could we reduce individual healthcare costs, but the NHS could also see substantial long-term savings. If a significant percentage of the population regularly engages in active travel, such as cycling with electric bikes, there would likely be:
- Fewer GP visits for preventable conditions like high blood pressure and diabetes.
- Lower costs for medications related to lifestyle diseases.
- Decreased need for costly surgeries and treatments resulting from inactivity-related illnesses.
Moreover, the reduction in pollution-related health problems and mental health issues due to increased active travel could further ease the strain on NHS resources, allowing funds to be allocated more effectively across the healthcare system.
Learning from the Netherlands: A Model for Active Travel
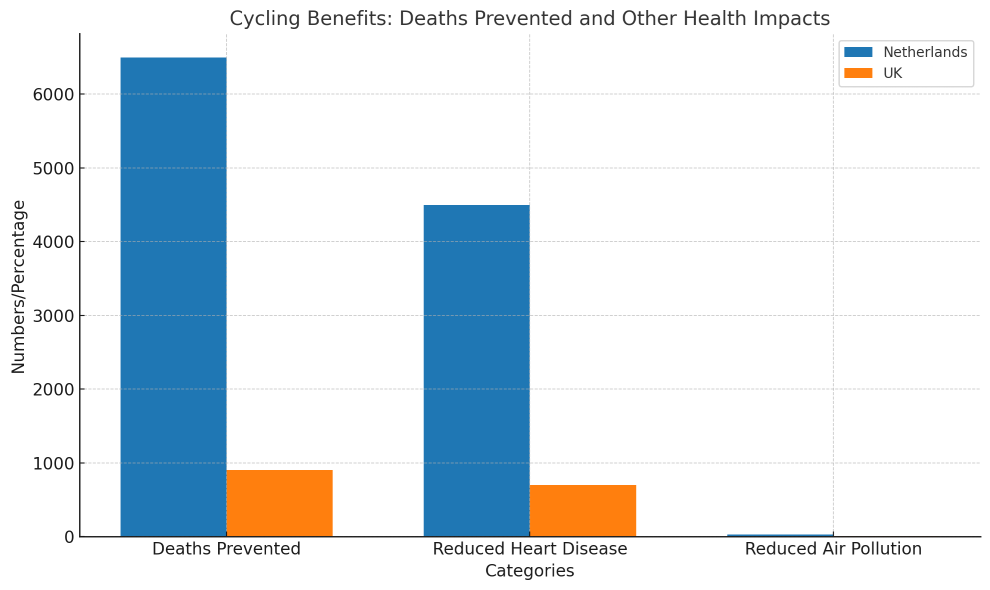
The UK can learn from countries like the Netherlands, where cycling is ingrained in the culture and healthcare outcomes reflect the benefits of active transport. The Dutch government has long prioritized cycling infrastructure, making it easier and safer for people of all ages to cycle regularly. As a result, 27% of all trips in the Netherlands are made by bike, compared to just 2% in the UK.
The impact on public health is significant. According to a study by the University of Utrecht, the widespread use of bicycles in the Netherlands prevents approximately 6,500 deaths annually and adds six months to the average life expectancy of the population. In addition to better physical health outcomes, the Netherlands also sees:
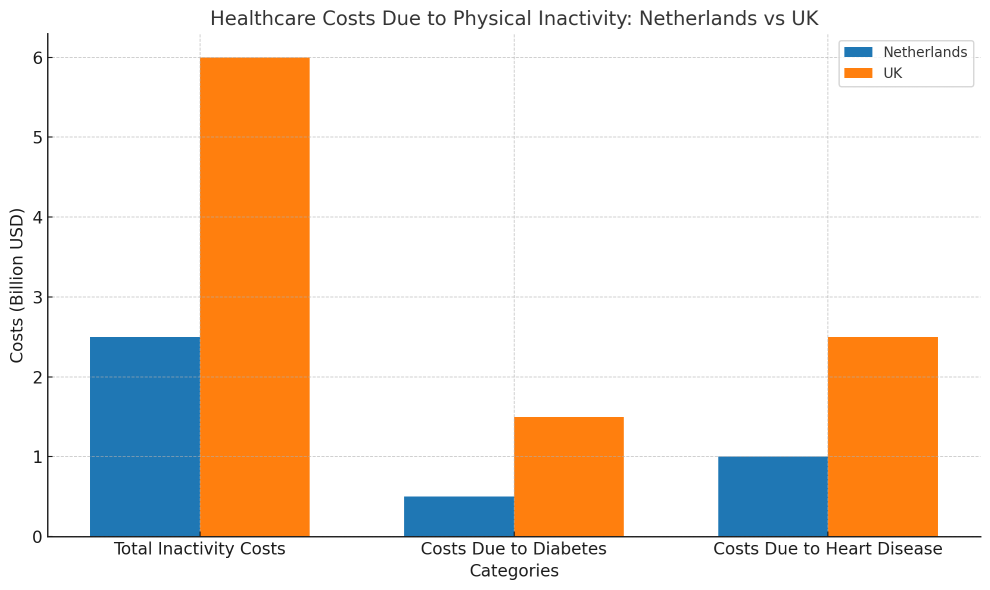
Here are some graphs showing how the UK is somewhat behind in health
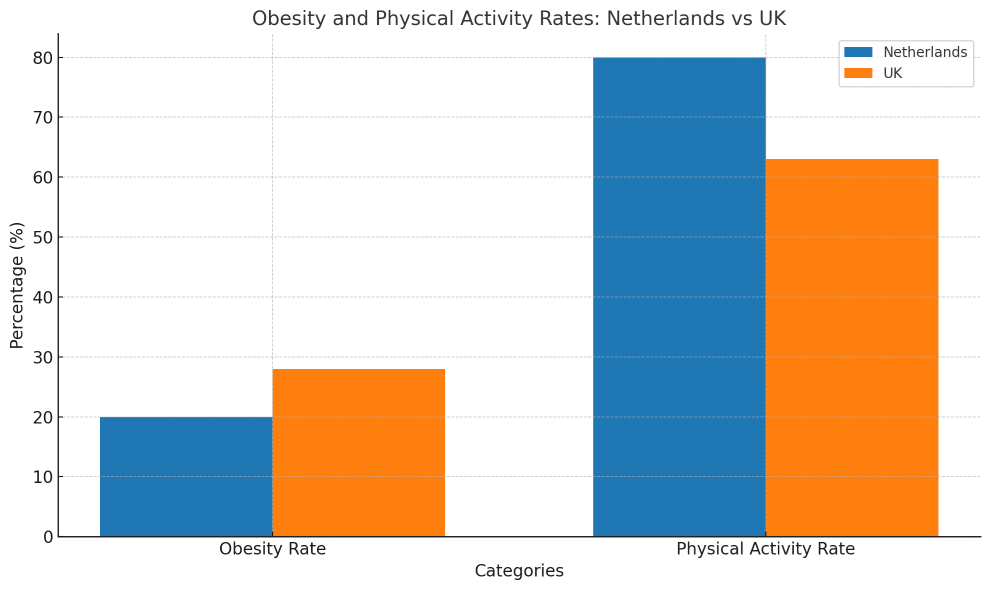
- Lower rates of obesity: The Dutch population experiences lower obesity rates compared to countries with higher car use.
- Fewer pollution-related illnesses: With more people cycling and walking, the country benefits from improved air quality, leading to fewer cases of respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD).
- Enhanced mental well-being: Regular physical activity through cycling has been shown to improve mental health, reducing anxiety, depression, and stress, which has a direct impact on lowering healthcare costs related to mental health interventions.
By adopting some of the policies and infrastructure seen in the Netherlands, the UK could not only improve public health but also significantly reduce the economic burden on the NHS. Encouraging electric bike use, as seen with subsidies and widespread availability in the Netherlands, could be a crucial step toward achieving these health and environmental benefits in the UK.
How does patient satisfaction in the Dutch healthcare system compare to that of the NHS?
Patient satisfaction in the Dutch healthcare system generally tends to be higher than that of the NHS, with surveys indicating that around 80% of Dutch patients report being satisfied with their care compared to approximately 70% of NHS patients. Factors contributing to this difference include shorter waiting times and a more personalized approach in the Netherlands, alongside a greater emphasis on patient-centered care. This comparison underscores the potential benefits of adopting similar strategies within the NHS to enhance patient experience and satisfaction.